May 2 2018
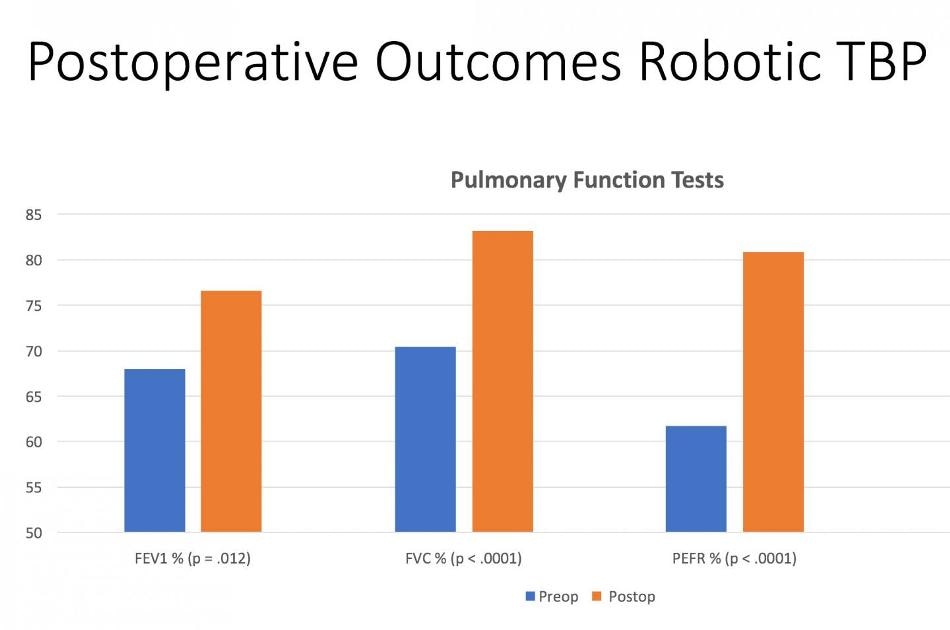 Postoperative outcomes in patients who underwent R-TBP at Lenox Hill Northwell Health, New York, N.Y. (Credit: Richard Lazzaro, MD)
Postoperative outcomes in patients who underwent R-TBP at Lenox Hill Northwell Health, New York, N.Y. (Credit: Richard Lazzaro, MD)
According to a research presented at the 98th Annual Meeting of the American Association for Thoracic Surgery, robot-assisted tracheobronchoplasty (R-TBP) can now be safely carried out, and it broadens the treatment options for patients suffering from tracheobronchomalacia, a high-risk, complex population. In contrast to the accepted treatment, this procedure is minimally invasive and the outcome was no mortality, low morbidity, and considerable improvement of the symptoms of patients.
Tracheobronchomalacia (TBM) is a disabling disease of the central airways with very little treatment options. Upon developing severe symptoms, tracheobronchoplasty is the accepted surgical option; however, it is performed only in very few chosen patients owing to its major risks for complications and death. TBM is caused due to damage or softening of the cartilaginous structures of the airway walls in the bronchi and trachea. Patients suffering from TBM experience persistent cough and breathing difficulties and are normally affected by pneumonia and other respiratory infections. Severe TBM results in complete or near complete destruction of the trachea.
TBM is a vastly underdiagnosed condition that has remained virtually untreated for decades. Its prevalence has been estimated to be as high as 10 percent in the general population, but data indicate that only 262 tracheoplasties were performed in the US between 2002 and 2017. A minimally invasive approach may expand the possibilities.
Richard Lazzaro, MD, Chief, Division General Thoracic Surgery, Lenox Hill Hospital
In 2013, the first minimally invasive, robot-assisted R-TBP was performed in the United States by Dr Lazzaro at Lenox Hill Hospital, New York, N.Y. to treat a patient with severe TBM. From that time, this method has been used to treat over 40 patients at the hospital. Data presented at the 98th AATS Annual Meeting assess the patient demographics, complications, surgical outcomes, and patient satisfaction.
Investigations of records of 435 patients with clinical suspicion of TBM who underwent dynamic CT scans from May 2016 to December 2017 were performed. TBM was defined as more than 50% destruction of the airway examined through CT scan. Of these patients, 145 were further assessed by thoracic surgery, and R-TBP was performed on 42 patients suffering from severe symptomatic TBM.
Pulmonary function tests at about four months following the surgery indicated considerable improvement in most of the patients. The tests revealed a considerable increase in the mean percent forced vital capacity (FVC) from 70.6% to 85.6% after performing R-TBP. Likewise, the mean preoperative percent predicted peak expiratory flow rate (PEFR) was 61.75% and increased to 80.85% following surgery. Immediate postoperative bronchoscopies were not needed in any patients, and no patients were reintubated. Postoperative complications were very less: two patients developed pneumothorax and one patient developed pneumonia. There were no deaths at 90 days following surgery, and all patients were discharged home.
Despite the fact that long-term patient follow-up is still progressive, 35 patients completed a five-point (Likert scale) postoperative survey evaluating satisfaction with the R-TBP procedure. More than 80% of patients reported satisfaction with the overall outcomes of the procedure, and most of them reported subjective improvement of shortness of breath, cough, and ability to manage respiratory infections.
These results show that R-TBP can be performed with low morbidity and mortality. Early follow-up reveals that most patients clearly see a dramatic relief in symptoms with a corresponding rise in pulmonary function tests. However, there are still many challenges to overcome. First and foremost is patient selection. A minority of patients do not have significant benefit, but reasons are often unclear.
Richard Lazzaro, MD, Chief, Division General Thoracic Surgery, Lenox Hill Hospital
More analyses are needed in relation to the optimal mesh size, role of stents, and tailored repair for distinctive malacic airway geometry. Further advanced imaging might help in better non-invasive diagnosis and operative planning.